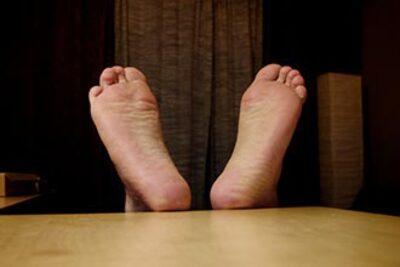
Dry feet diabetes is a common condition seen among individuals living with diabetes. It’s a manifestation of the broader complications that can arise due to uncontrolled blood sugar levels. As many diabetic patients often face issues related to dry skin, moisture retention becomes a significant concern. This article delves into the various dimensions of dry feet diabetes, shedding light on its causes, implications, and management strategies.
Table of Contents
The Connection Between Diabetes and Skin Health

Diabetes can lead to several skin conditions, and dry feet are among the most prevalent. When the body struggles to maintain stable glucose levels, it affects skin health in several ways.
High Blood Sugar Levels and Skin Hydration

High blood sugar levels often result in dehydration, which affects the skin’s ability to retain moisture.
Diabetic patients tend to experience increased urination as the kidneys work overtime to filter excess sugar from the bloodstream. This can lead to fluid loss, resulting in dry skin and particularly dry feet.
Additionally, when the skin lacks moisture, it becomes more prone to cracks and fissures. These openings can serve as gateways for infections, making foot care crucial for those with diabetes.
Neuropathy and its Impact on Foot Care
Another critical aspect of diabetes-related foot health is peripheral neuropathy, a condition resulting from nerve damage due to high blood sugar levels.
This condition can diminish sensation in the feet, leading individuals to be unaware of injuries or infections. A lack of feeling may cause a person to overlook signs of dry skin or cracks, which could worsen over time if not treated.
Poor Circulation and Healing
Diabetes can also lead to poor circulation, further complicating foot health.
Reduced blood flow means that any existing wounds or cracks will heal more slowly, leading to an increased risk of infection. Consequently, maintaining healthy, moisturized feet becomes vital for those diagnosed with diabetes, as it aids in preventing complications stemming from dry skin.
Effective Management Strategies for Dry Feet Diabetes

Managing dry feet diabetes encompasses several proactive measures that aim to keep the feet hydrated and healthy.
Regular Moisturizing Practices
The importance of hydration cannot be overstated when managing dry feet diabetes.
Using a good quality moisturizer specifically designed for feet is essential. Look for products containing urea, glycerin, or lactic acid, as they can significantly improve moisture retention.
It’s best to apply lotion after bathing or showering, as this locks in moisture. However, ensure that the cream does not get between the toes, where excess moisture can foster fungal infections.
Routine Foot Inspections
Regularly inspecting your feet is crucial for early detection of any complications.
Examine your feet daily for cuts, blisters, redness, or any other irregularities. For those with neuropathy, using a mirror can help spot areas that might otherwise go unnoticed.
If you notice signs of dryness, such as scaling or cracking, address these immediately. Dealing with minor issues promptly can prevent them from escalating into severe problems down the line.
Choosing Appropriate Footwear
Proper footwear plays an integral role in managing dry feet diabetes.
Opt for shoes that provide adequate support and cushioning to minimize friction and pressure points. Avoid tight-fitting socks and shoes, as these can exacerbate dryness and lead to blister formation.
Additionally, breathable materials that allow for airflow can help maintain moisture levels without causing excessive sweating.
Lifestyle Changes to Alleviate Dry Feet Diabetes

Making lifestyle adjustments can significantly influence the degree of dryness experienced by diabetic patients.
Diet and Nutrition
Nutrition is a cornerstone of diabetes management, influencing both blood sugar levels and skin health.
Incorporating plenty of vegetables, fruits, whole grains, and lean proteins can optimize overall health. Foods rich in omega-3 fatty acids, such as salmon and walnuts, can improve skin elasticity and hydration.
Moreover, staying adequately hydrated by drinking enough water and reducing consumption of sugary drinks can prevent dehydration—a contributing factor to dry skin.
Regular Exercise
Engaging in regular physical activity is beneficial for improving circulation, which is essential for maintaining skin health.
Whether it’s walking, cycling, or swimming, exercise stimulates blood flow to the extremities, promoting nutrient delivery and waste removal. Improved circulation can enhance the healing processes within the body, thereby reducing instances of dry feet.
Stress Management Techniques
Stress can have numerous negative effects on the body, including exacerbating symptoms associated with diabetes.
Implementing stress-reduction techniques such as yoga, meditation, or even simple breathing exercises can aid in better blood sugar control. Improved stress management can indirectly promote healthier skin through better hormonal regulation and balanced glucose levels.
FAQs

What causes dry feet in diabetics?
Dry feet in diabetics primarily stem from high blood sugar levels, leading to dehydration and reduced sensation due to neuropathy. Poor circulation further aggravates the condition.
How can I prevent my feet from drying out?
To prevent dry feet, regularly moisturize them, inspect for cuts or cracks, wear appropriate footwear, and maintain proper blood sugar levels through diet and exercise.
Is it safe to use foot scrubs or exfoliants?
Foot scrubs or exfoliants should be used cautiously. If you have sensitive skin or existing foot conditions, consult a healthcare provider before using these products.
What are the signs of infection in dry feet?
Signs of infection include increased redness, swelling, warmth, pus discharge, and persistent pain. If any of these occur, seek medical attention immediately.
Can diabetes cause changes in nail health?
Yes, diabetes can lead to nail abnormalities such as thickening, discoloration, or fungus infections. Regular foot care and monitoring can help mitigate these issues.
Conclusion
Living with dry feet diabetes requires vigilance, awareness, and proactive management. By understanding the relationship between diabetes and skin health, individuals can implement effective strategies to maintain moisture and prevent complications. Through routine foot inspections, proper moisturizing practices, and lifestyle adjustments, one can significantly reduce the risks associated with dry feet. By taking charge of one’s foot health, the journey with diabetes can become a little easier, allowing for improved quality of life and well-being.