Care for diabetic foot ulcer is a crucial aspect of managing diabetes, as it can prevent serious complications that may arise from untreated wounds. Diabetic foot ulcers are common among individuals with diabetes due to poor circulation and nerve damage, making proper care essential for healing and overall health. Through diligent attention to foot hygiene, regular monitoring, and timely medical intervention, individuals can significantly reduce the risks associated with diabetic foot complications.
As we delve into the world of care for diabetic foot ulcer, we will explore various methods and insights that can enhance healing processes, empower patients, and improve quality of life.
Table of Contents
Understanding Diabetic Foot Ulcers

A comprehensive understanding of diabetic foot ulcers is the foundation for effective care. These ulcers often result from a combination of factors related to diabetes, including neuropathy and peripheral vascular disease.
Causes of Diabetic Foot Ulcers

The causes of diabetic foot ulcers are multifaceted, stemming primarily from complications associated with high blood sugar levels.
One significant factor is peripheral neuropathy, which damages nerves in the feet. This condition reduces sensation, meaning that injuries or pressure sores can go unnoticed. As a result, these seemingly minor injuries may develop into painful ulcers over time.
Poor circulation is another critical player in the development of foot ulcers. Diabetes can lead to narrowing of blood vessels, restricting blood flow to the extremities. This compromised circulation hampers the body’s ability to deliver oxygen and nutrients necessary for tissue repair, making healing sluggish and increasing the risk of infection.
Risk Factors Associated with Diabetic Foot Ulcers
Identifying risk factors is key to preventing diabetic foot ulcers. Not everyone with diabetes will develop foot ulcers, but certain characteristics heighten the risk.
Individuals with a history of foot ulcers or amputations have a higher likelihood of recurrence. Additionally, poor blood sugar control accelerates the onset of complications throughout the body, including the feet. Lifestyle choices, such as smoking and obesity, can exacerbate these conditions further.
Regular foot assessments by healthcare professionals are also vital. Those with visual impairments or limited mobility may not notice early signs of ulceration, highlighting the need for proactive measures in foot care.
Symptoms of Diabetic Foot Ulcers
Recognizing symptoms is an essential part of care for diabetic foot ulcer. Early detection often leads to better outcomes. Key symptoms may include:
- A visible sore or wound on the foot
- Redness or swelling around the lesion
- Unusual warmth in the affected area
- Discharge or an unpleasant odor emanating from the ulcer
Promptly addressing any unusual changes in foot health can be the difference between a minor inconvenience and a major health crisis.
Effective Care Strategies for Diabetic Foot Ulcers

Once a diabetic foot ulcer has developed, appropriate care strategies must be implemented immediately to promote healing and avoid complications.
Proper Wound Cleaning Techniques
Effective cleaning techniques form the backbone of care for diabetic foot ulcer. Regularly cleaning the wound helps remove debris and bacteria that can lead to infections.
Start by gently rinsing the ulcer with mild soap and warm water. Avoid using harsh antiseptics, as they might irritate the exposed tissues. After cleaning, pat the area dry with a clean towel. If possible, air drying can also aid in the healing process.
Applying a sterile dressing after cleaning serves dual purposes: it protects the ulcer from additional injury and keeps the area moist to foster healing. Changing the dressing regularly based on the doctor’s advice ensures that any exudate is managed properly and that the wound is monitored closely for signs of infection.
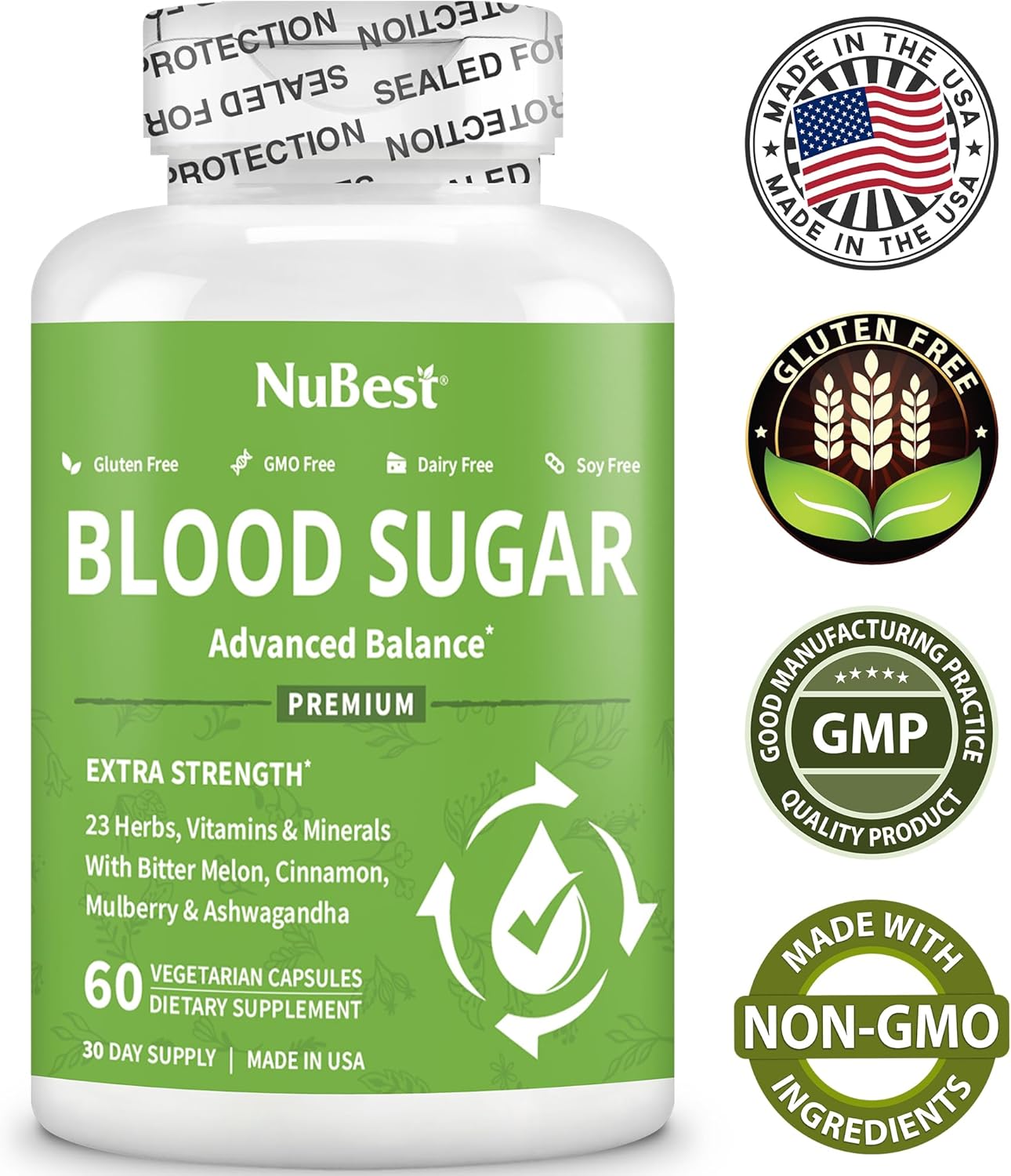
Monitoring Blood Sugar Levels
To effectively manage a diabetic foot ulcer, maintaining stable blood sugar levels is crucial. Fluctuations in glucose can significantly impact the healing process, leading to prolonged recovery times.
Implementing a consistent monitoring routine allows individuals to identify trends in their blood sugar readings. It empowers them to make necessary adjustments to their diet, physical activity, and medication regimen. For instance, if readings are consistently high, consulting a healthcare provider to reevaluate treatment options may prove beneficial.
Seeking Professional Medical Assistance
Medical intervention is paramount for ulcers that do not show signs of improvement despite proper self-care efforts. Healthcare professionals can provide valuable insights, prescribe antibiotics if an infection is identified, and recommend specialized dressings or therapies.
Additionally, podiatrists may suggest custom footwear or orthotics to alleviate pressure on the ulcer. Having a multidisciplinary approach to care enhances the chances of successful healing.
Lifestyle Modifications for Prevention

Preventing diabetic foot ulcers goes beyond direct care; lifestyle modifications play a pivotal role in minimizing risks and ensuring optimal foot health.
Maintaining Foot Hygiene
Proper foot hygiene is one of the simplest yet most effective preventative measures. Daily inspections of feet for any cuts, blisters, or redness can help catch problems before they escalate.
Individuals should wash their feet daily in warm water, ensuring to dry thoroughly, especially between the toes where moisture can linger. Regular nail trimming can prevent ingrown toenails, which can lead to pain and potential ulcer formation.
Choosing Appropriate Footwear
Choosing the right footwear cannot be overstated. Ill-fitting shoes can contribute to pressure points and create opportunities for ulcers to develop.
Aim for well-fitted shoes with enough room to accommodate foot swelling. Consider orthotic inserts if recommended by a healthcare professional. Avoid walking barefoot, even at home, to minimize the risk of cuts or scrapes.
Staying Active and Managing Weight
Physical activity plays a vital role in managing both diabetes and foot health. Regular exercise improves circulation and can aid in weight management—both of which are essential in reducing the risk of developing diabetic foot ulcers.
Engaging in low-impact exercises, like swimming or cycling, minimizes stress on the feet while still reaping the benefits of physical activity. Additionally, combining exercise with a balanced diet contributes to overall wellness, helping maintain healthy blood sugar levels.
Conclusion

In conclusion, care for diabetic foot ulcer encompasses a holistic approach involving vigilant monitoring, effective wound care, and proactive lifestyle modifications. Understanding the causes, risk factors, and symptomatology of diabetic foot ulcers equips individuals to take charge of their foot health.
By implementing practical strategies—such as maintaining hygiene, monitoring blood glucose levels, and seeking timely medical intervention—individuals can significantly mitigate the risks associated with diabetic foot complications. As the saying goes, prevention is better than cure; therefore, investing in foot care today can lead to healthier tomorrows.